Obesity is not just a personal health issue in America—it is a national epidemic. According to the Centers for Disease Control and Prevention (CDC), over 41.9% of U.S. adults are obese as of 2021–2022, and the rate continues to climb. This condition affects every aspect of life—from increased risk of disease and death to significant healthcare costs and economic burdens.
Defining Obesity: What It Really Means
Obesity is commonly determined using Body Mass Index (BMI), where:
A BMI of 25–29.9 = Overweight
A BMI of 30 or more = Obese
BMI is not perfect—it doesn’t account for muscle mass or fat distribution—but it remains a widely used tool for population-level analysis.
Obesity in the United States: By the Numbers
National Overview
Adults: 41.9% are obese (CDC, NHANES 2021–2022)
Children/Teens (2–19 years): 19.7% are obese
Severe Obesity (BMI ≥ 40): 9.2% of adults
Obesity by Race and Ethnicity
Non-Hispanic Black adults: 49.9%
Hispanic adults: 45.6%
Non-Hispanic White adults: 41.4%
Non-Hispanic Asian adults: 16.1%
Obesity is also strongly linked with income and education levels. Lower-income groups and those with less education tend to have higher obesity rates, often due to limited access to nutritious food and exercise options.
Obesity by State: Where the Problem Is Worst?
According to the CDC’s Behavioral Risk Factor Surveillance System (BRFSS) data for 2022:
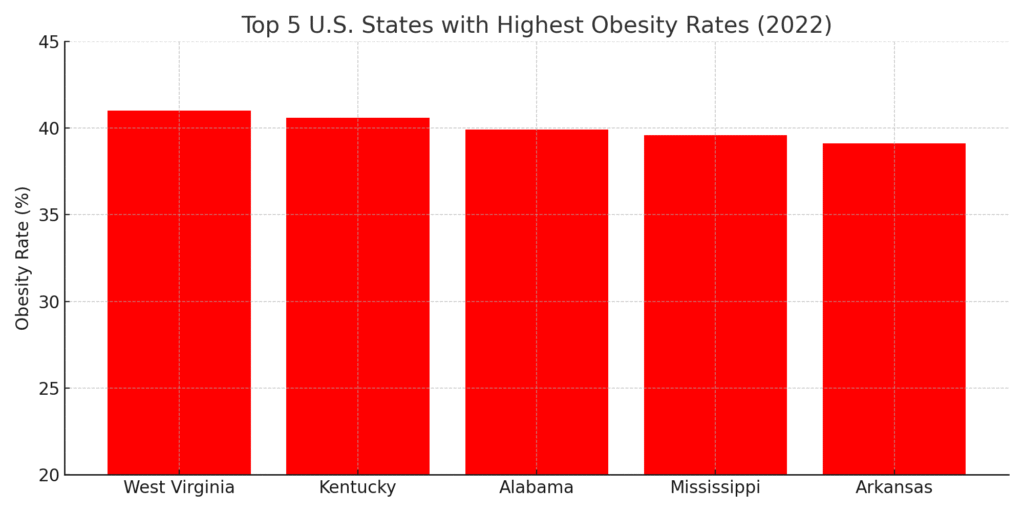
States with the Highest Obesity Rates
West Virginia – 41.0%
Kentucky – 40.6%
Alabama – 39.9%
Mississippi – 39.6%
Arkansas – 39.1%
These are primarily Southern states where obesity is linked to:
High consumption of fried, processed foods
Sedentary lifestyles
Economic challenges and poor access to healthcare
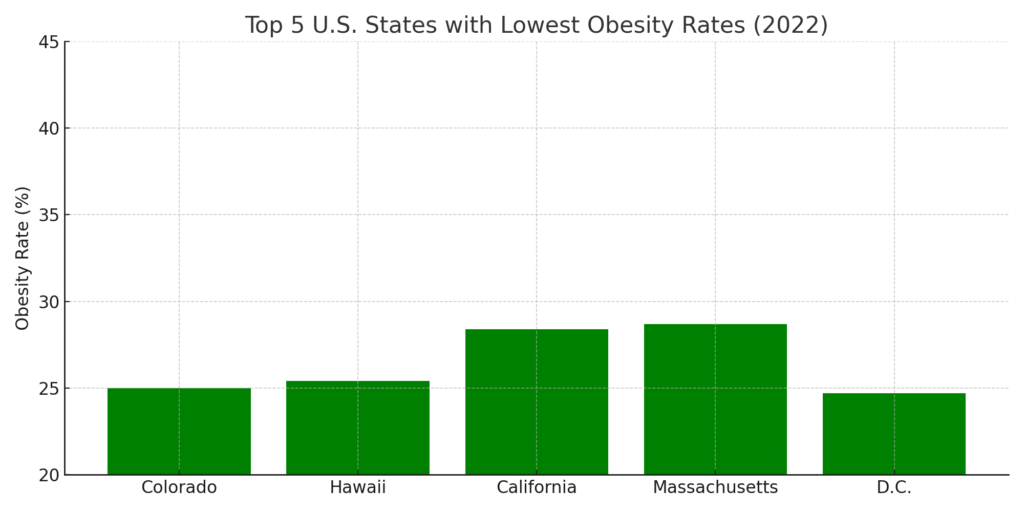
States with the Lowest Obesity Rates
Colorado – 25.0%
Hawaii – 25.4%
California – 28.4%
Massachusetts – 28.7%
Washington D.C. – 24.7%
These areas benefit from:
Higher rates of physical activity
Greater health awareness
Urban planning that encourages walking and cycling
Easier access to fresh produce and health services
Obesity by City: The Best and Worst
Cities with the Highest Obesity Rates
Data from the State of Obesity report by the Trust for America’s Health:
McAllen, Texas – Over 44% adult obesity rate
Memphis, Tennessee
Mobile, Alabama
Shreveport, Louisiana
Jackson, Mississippi
These cities often rank low in exercise levels and healthy food access.
Cities with the Lowest Obesity Rates
Boulder, Colorado – ~15% adult obesity rate
Honolulu, Hawaii
San Francisco, California
Seattle, Washington
Portland, Oregon
These cities are known for walkable neighborhoods, active lifestyles, and greater public health investment.
Why Is Obesity So Prevalent in America?
1. Diet and Food Culture
Fast food culture and oversized portions
High availability of ultra-processed foods
Sugar-laden beverages and snacks
2. Physical Inactivity
Less than 23% of Americans meet national exercise guidelines
Urban sprawl, screen addiction, and sedentary jobs contribute
3. Socioeconomic Inequality
“Food deserts” in urban and rural poor communities
Cheap, unhealthy food is more accessible than fresh produce
4. Mental Health
Emotional eating and food addiction are common
Depression and anxiety often correlate with weight gain
5. Medical and Genetic Factors
Thyroid disorders, PCOS, and insulin resistance
Some people may have a genetic predisposition to obesity
Health Consequences of Obesity
Type 2 Diabetes
Cardiovascular Disease
Certain Cancers (e.g., breast, colon, pancreatic)
Fatty Liver Disease
Osteoarthritis
Stroke and Sleep Apnea
According to a Harvard School of Public Health study, obesity increases the risk of early death by 20–30%, especially for those under 45.
Economic Cost of Obesity
Annual obesity-related healthcare costs in the U.S.: $173 billion
Employers lose billions due to absenteeism and reduced productivity
Public health systems bear the long-term burden of chronic illness
Scientific Research and Treatment Options
1. Lifestyle Change Programs
Diabetes Prevention Program (DPP): Showed a 5–7% weight loss reduces diabetes risk by 58%
Behavior therapy, food journaling, and regular coaching improve outcomes
2. Medications
FDA-approved drugs like semaglutide (Wegovy) and tirzepatide (Zepbound) show promising weight loss results (up to 15–20% reduction)
3. Bariatric Surgery
Recommended for BMI ≥ 40 or ≥ 35 with comorbidities
Roux-en-Y gastric bypass and sleeve gastrectomy are most common
Can lead to sustained 25–35% weight loss
4. Public Policy
Soda taxes in Berkeley, Philadelphia led to 20–25% reduced consumption
Menu labeling laws encourage better choices
Active transportation projects (bike lanes, parks) promote movement
How to Fight Obesity in America
Individual Strategies
Regular exercise (150 minutes/week minimum)
Whole-food, plant-based diet high in fiber and protein
Mindful eating and mental health support
Community and Government Initiatives
Redesigning school lunch programs
Urban planning that supports walking and biking
Public health campaigns on portion control and sugar intake
Incentives for grocery stores in underserved areas
Conclusion
Obesity is a multifaceted and deeply entrenched issue in American life. It varies widely by state, city, income, and race, reflecting systemic challenges as much as individual choices. While the numbers are staggering, there is hope through science, education, and policy reform.
To reverse the obesity epidemic, America must address root causes—from food systems to city planning—and build an environment that makes healthy living the easy choice for everyone.